Ivan Gerdzhikov
Department of Prosthetic dentistry, Faculty of Dental Medicine, Medical University of Sofia ivan_ger1971@abv.bg
Abstract: Introduction: The increased frequency of cancer diseases in the maxillofacial area rise the number of patients with maxillary resection, which leads to creating of different treatment methods.
Aim: The described clinical case follows up the opportunities of prosthetic treatment in patient with partial maxillectomy and evaluates the treatment effect of feeding and speaking restoration.
Material and methods: A prosthetic treatment of 63-years-old female patient with maxillary defect after oncological operation was conducted. There were preserved teeth 11, 12, 21 in the upper jaw and from 35 until 44 in the lower jaw. The treatment plan included the fabrication of post resection denture in the upper jaw and partial denture in the lower jaw. The impressions were taken with irreversible hydrocolloid impression material. The occlusion height and centric relations were fixed by baseplates and occlusal wax rims. Post resectioned denture was made with thick obturation part. Metal clasps were used in both dentures for providing retention and stability.
Results: The prosthetic treatment led to successful defect obturation and helped for speaking and feeding restoration.
Conclusion: The application of prosthetic treatment methods in patients with maxillary resection allows successful restoration of the damaged functions, which improves significantly their life quality. Keywords: oral cancer, maxillary resection, obturator, post resection denture.
Medical sciences and Health
- INTRODUCTION
Increased level of cancer diseases in maxillofacial area leads to higher number of patients with maxillary resection (1). The investigations (2) show a trend of their accumulation. This is the reason why oral cancer is one of the most common diseases in many countries after lymphoma and leukemia (3). A quadruple increased morbidity gives grounds to Suba et al. (4) to determined oral cancer as a disease of 21st centuries. Very often the patients go into hospital in the 3-4 stage, which makes the surgical treatment difficult (1,5,6). Despite of that, the researches revealed increasing of patients’ life expectancy aftermaxillary resection (7, 8). Damages, occurred after maxillary resection caused serious problems in chewing, swallowing, speaking and breathing (9, 10, 11). The state of functional disorders correlates mainly with the defect’s size and localization (12, 13). The data shows less functional disorders in patient with small defects and preserved teeth (14, 15). According to Devlin et Barker (16), the defect size and localization, such as the condition of the preserved teeth, are determinative for the state of disorder and prognosis. This thesis is confirmed by other surveys, which report lower average values damaged speech and chewing n patients with larger defects (17).
Prosthetic treatment methods take main role in the complex treatment and rehabilitation of patients with maxillary resection (18, 19, 20). Most of the authors (19, 21, 22) perform prosthetic rehabilitation after maxillectomy in three stages – with surgical, temporary and definitive obturator. Each construction has its own specific, which affects life quality in different way (9, 23). The application of three-stage treatment method allows restoration of feeding, speaking, patients’ aesthetic and provides permanent good life-quality (9, 19, 21).
2. AIM
The described clinical case follows up the opportunities of prosthetic treatment in patient with partial maxillectomy and evaluates the treatment effect of feeding and speaking restoration.
3. MATERIALS AND METHODS
It is described a prosthetic treatment of 63-years-old female patient with maxillary resection as a result of oncological operation. The intraoral examination revealed the presence of communication between the oral and nasal cavity, which involved the left side of the maxilla and reached the soft palate (fig.1). Teeth 11, 12, 21 were covered by single crowns and preserved. The lower jaw has had teeth from 35 until 44. The patient complained, that two months after the operation she was still unable to speak and eat. There were additional difficulties, caused by
painful and limited mouth opening. These problems had become more serious in the last month, because of conducted radiotherapy.


A treatment plan was compiled, which involved the fabrication of post resection upper partial denture. The impressions of both jaws were taken with standard trays and irreversible hydrocolloid impression material. The defect was covered with gauze tamponade, in advance. Gypsum master models were cast in the laboratory and baseplates with occlusal rims were fabricated (fig.2). The occlusal height and centric relations were fixed in the next clinical stage. After successful trial denture, the post resectioned denture was fabricated by heat-cured acrylic resin with low quantity of residual monomer. The substitution part of the denture was fabricated as a hollow bulb obturator, due to defect’s size and localization. Single clasps were used for providing retention and stability (fig.3). These types of retainers were used for the lower partial denture. Polished and disinfected dentures were adjusted and articulated in patient’s mouth in the final clinical appointment. Numerous retentive places in defect area were the reason for many appointments for treatment of decubitus wounds.

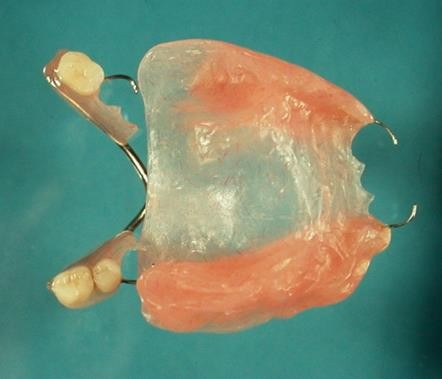
Fig. 3. Finished dentures – occlusal (a), palate (b) point of view
4. RESULTS
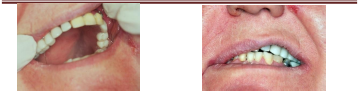
The results of the performed treatment showed successful restoration of damaged functions. It was achieved an optimal retention and stability of the upper denture (fig.3). The fabrication of hollow bulb obturation part created a barrier between the oral and nasal cavity. The specific defect localization, on the border of soft palate, had been created a rick of bad hermetization, but these concerns were not justified. Patient’s speaking was restored immediately after the treatment, as expected. The occlusal relations, chewing and feeding were recovered, as well (fig. 4). The patient was very satisfied, that she was able to drink liquids and could swallow. All these positive changes after the prosthetic treatment improved her self-esteem and life quality.
5. DISCUSSION
The prosthetic treatment in patients with maxillary resection is correlated with many difficulties. The main problems in the described clinical case were connected with limited mouth opening and defect’s localization on the soft palate border. The performed radiotherapy was a problem, as well. Due to these factors, series of exercise were conducted for overcoming the trismus and relaxation of the masticatory muscles. All these efforts allowed successful impression registration from the jaws. This method is recommended by some authors, as the only option for achieving good results in the prosthetic treatment of patient with maxillary resection (19). The limited oral opening was the reason for fabrication a hollow bulb obturator with thick substitution part, which facilitates the right placing in the mouth. This provided the needed hermetization and gave stability to the denture. The natural preserved teeth were used for better retention, which is a common technique in this type of treatment (12, 13, 15). The application of a hollow bulb obturator restored patient’s swallowing and ability to drink liquids. Speaking and feeding recovery confirmed the efficiency of the prosthetic treatment and the state of many authors, that the prosthetic methods are the main treatment options for patient with maxillary resection (18, 19, 20).
6. CONCLUSION
The application of prosthetic treatment methods in patients with maxillary resection allows successful restoration of the damaged functions, which improves significantly their life quality.
REFERENCES
- Lung, T., O. Tăşcău, H. Almăşan, O. Mureşan. Head and neck cancer, epidemiology and histological aspects
– Part 1: a decade’s results 1993-2002. J. Craniomaxillofac. Surg., 2007, Mar, 35 (2), 120-125
- Wen, Y., X. Dai, C. Wang, L. Li, F. Fu, X. Wang, X. Tang, H. Liu, C. Hua, J. Pan. A retrospective clinical study of 6539 cases of malignant oral-maxillofacial tumors. Hua Xi Kou Qiang Yi Xue Za Zhi, 2001, Oct, 19 (5), 296-299.
- Al-Balawi, S. A., A. Nwoku. Management of oral cancer in a tertiary care hospital. Saudi Med. J., 2002, Feb, 23 (2), 156-159.
- Suba, Z., S. Mihályi, D. Takács, S. Gyulai-Gaál. Oral cancer: morbus Hungaricus in the 21st century. Fogorv. Sz., 2009, Apr, 102 (2), 63-68.
- Kovács, A. F., W. Megahed, M. Scholz, R. Sader. Survival improvement of a unicentric overall population in
20 years: 1038 patients with oral and oropharyngeal squamous cell cancer 1983-2004. Mund Kiefer Gesichtschir, 2007, Nov, 11 (5), 267-283.
- Vartanian, J. G., L. Kowalski. Acceptance of major surgical procedures and quality of life among long-term survivors of advanced head and neck cancer. Arch. Otolaryngol. Head Neck Surg., 2009, Apr, 135 (4), 376- 379.
- Lethaus, B., N. Lie, F. de Beer, P. Kessler, C. de Baat, H. Verdonck. Surgical and prosthetic reconsiderations in patients with maxillectomy. J. Oral Rehabil., 2010, Feb, 37 (2), 138-142.
- Rogers, S. N., J. Brown, J. Woolgar, D. Lowe, P. Magennis, R. Shaw, D. Sutton, D. Errington, D. Vaughan. Survival following primary surgery for oral cancer. Oral Oncol., 2009, Mar, 45 (3), 201-211.
- Depprich, R., C. Naujoks, D. Lind, M. Ommerborn, U. Meyer, N. Kübler, J. Handschel. Evaluation of the quality of life of patients with maxillofacial defects after prosthodontic therapy with obturator prostheses. Int.
J. Oral Maxillofac. Surg., 2011, Jan, 40 (1), 71-79.
