Ivan Gerdzhikov, Department of Prosthetic dentistry, Faculty of Dental Medicine, Medical University – Sofia, Bulgaria.
ABSTRACT:
Aim: The aim of the described method is to present the main stages in the prosthetic treatment with hollow bulb obturator, which provides optimum defect hermetization and restoration of the damaged functions.
Materials and methods: The clinical case, de- scribed is on a 70-years-old patient with edentulous jaws and maxillary defect in the right half of the upper jaw. The preliminary impressions were taken with irreversible hydrocolloid impression material, and the final impres- sions were taken with additive silicone material. The oc- clusion height and the centric relations were registered as the classical technique. After the successful trial den- ture appointment, the surface of the plaster master model was covered by isolation polish. After this procedure, the master model was covered by even wax layer with 5mm thickness. It was designed to be thinner in the area of the resection line. The designed cavity was filled in with sili- cone impression material and covered with the folio. The baseplate with the arranged teeth was fixed to the model, packed in the cuvette and finished from heat-cured acrylic resin with low quantity of residual monomer. After the po- lymerization process, the silicone material was removed, and the obturator’s cap was fixed to the denture’s base- plate with cold cured acrylic resin. The obturator and the complete denture of the mandible were adjusted and ar- ticulated in patient’s mouth in the final clinical stage.
Results: The applied prosthetic method allowed successful defect hermetization and helped for the resto- ration of the speech, feeding and patient’s self-esteem.
Conclusion: Prosthetic rehabilitation of patients with maxillary resection is possible only with the appli- cation of specific treatment methods.
Keywords: maxillary resection, maxillary defect, obturator, post resection denture.
INTRODUCTION
Surgical treatment of cancer in the oral cavity causes severe damages of patients’ feeding, speech and swallowing [1]. The main aim of the prosthetic rehabili- tation is the restoration of the functions and improvement of the life quality [2]. Different methods and materials are applied, despite the defect’s size, location and the pres- ence of preserved teeth [3]. The treatment plan should be pursuant to the main prosthetic principles and individual characteristics, as well [4, 5]. It is necessary to take into account all the factors, which affect denture’s retention and stability [6].
According to Devlin et Barker [7], the specificity of maxillofacial disorders needs the application of spe- cial treatment methods. This is correlated with the usage of new impression techniques [8, 9] and occlusal closure registration [10]. Despite that, Zaki et Aramany [11] sug- gest classical impression techniques, used in the fabrica- tion of complete dentures.
Numerous of methods, with different materials and technologies, for fabrication of definitive obturators are described [12, 13, 14, 15, 16, 17]. Some authors consider, that complete hermetization can be achieved only with closed hollow bulb obturators [18, 19]. The obturation part is formed by a gypsum core, fixed to the cast model before flasking [20]. An alternative method exists, in which the hollow part is formed from silicone material [21], ice [22], sugar [23], asbestos [19], pumice [24] and plate from pure acetate [25].
Many authors [24, 26] claim that optimal defect hermetization could be reached only with the step-by-step fabrication of the obturation part and the baseplate, but others [27, 28] suggest the application of shortened meth- ods. Specific methods are applied too, in which the tem- porary obturator turns in permanent [14].
According to most authors [17, 29, 30], the treat- ment with hollow bulb obturators is connected with many difficulties, which had their substitute with opened bulb obturators. Their main advantage is the reduction of the weight- from 6,55% to 35,06% less than the solid obturators [30]. Electromyographic examinations revealed better clinical results in the application of opened bulb obturator with substitute part [29]. This is explained with the reduced weight and volume, which facilitates the in- sertion in the defect and provides better comfort for the patient [17]. The main disadvantage of the opened obturators is the difficult cleaning [31].
AIM
The aim of the described technique is to present the main stages in the prosthetic treatment of patients with partial maxillectomy and a method of fabrication of closed hollow bulb obturator, which can provide optimal defect hermetization and restoration of the damaged functions.
MATERIALS AND METHODS
The clinical case reports the prosthetic treatment of a 70-years-old patient with a maxillary defect as a re- sult of a cancer operation. The intraoral examination re- vealed a unilateral defect in the right side of the upper jaw, which reach the midline and the soft palate [Fig.1]. There are no preserved teeth in both jaws. Facial asym- metry and right cheek sagging are visible [Fig.2].

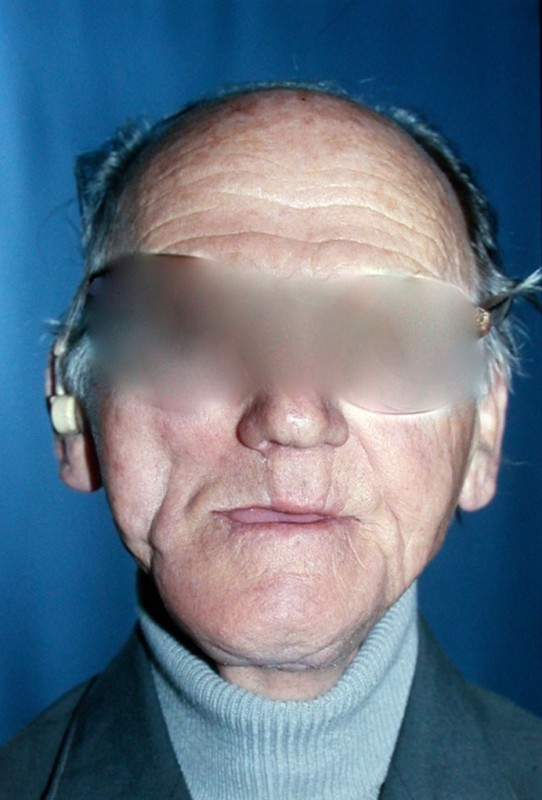
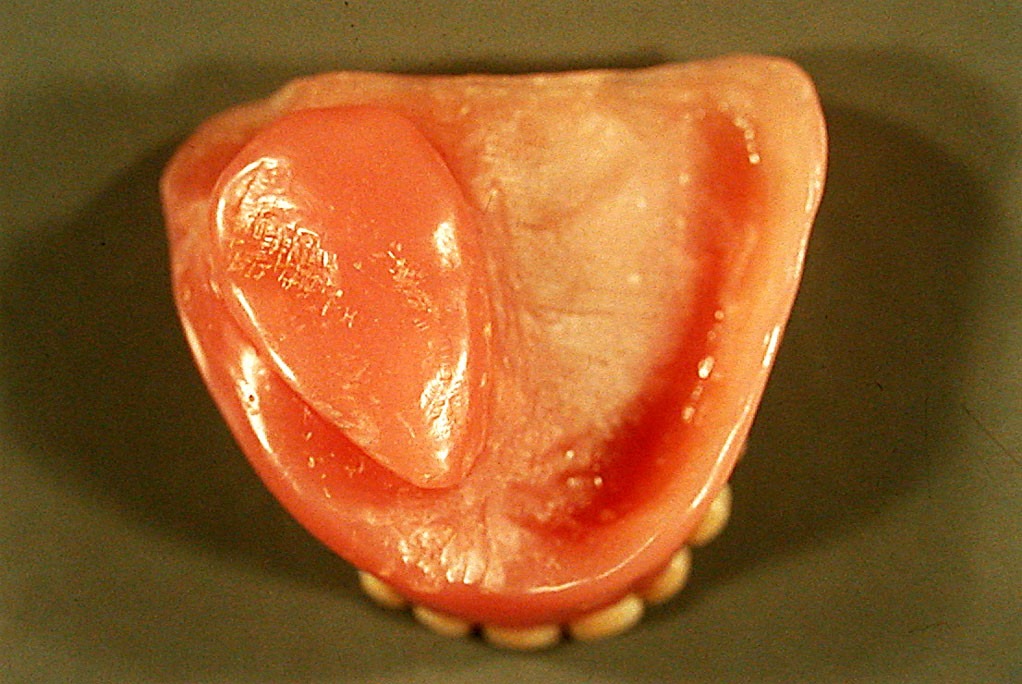
The treatment plan included the fabrication of closed hollow bulb obturator and a complete denture for the lower jaw. The prosthetic rehabilitation was con- ducted in 5 clinical stages. The preliminary impressions from irresistible hydrocolloid material were taken with standard metal trays in the first clinical stage. The defect of the upper jaw was tamped with gauze in advance. Individual trays from light-cured acrylic resin were made in the dental laboratory, with which the final impressions were taken with additive silicone in the second clinical stage. The occlusion height and the centric relations were fixed in the third appointment. The denture was sent to the laboratory for final completion after the successful trial denture in the fourth appointment. In this laboratory stage, preparation of the gypsum model for flasking was made. The surface in the defect area was covered with isolation polish, and the cavity was covered with an equal layer of wax with a thickness of 5mm, which was thinner in the area of the resection line. The substitution part was filled in with silicone impression material and covered with foil [Fig. 3]. The baseplate with the arranged teeth was fixed carefully to the model, flasked into a cuvette and completed by heat-cured acrylic resin with low quan- tity of residual monomer. After the polymerization process, the silicone material was removed, and the obturator’s cap was fixed to the denture’s baseplate with cold cured acrylic resin [Fig. 4]. The obturator and the complete denture of the mandible were adjusted and articulated in patient’s mouth in the final clinical stage [Fig. 5].


RESULTS
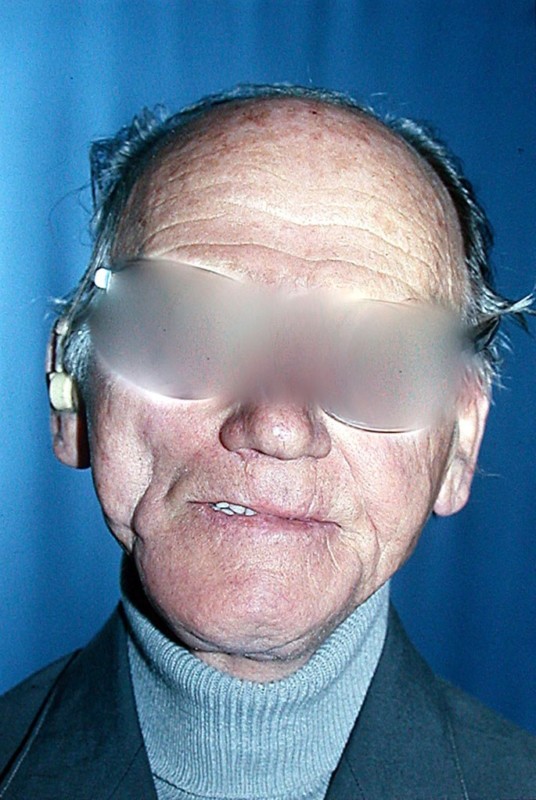
The results from the treatment revealed successful defect hermetization and creating a barrier between the oral and nasal cavity, which was the main aim of the prosthetic treatment. The tightly defect obturation allows the ability for fully speaking restoration and patient’s social life. The complex prosthetic rehabilitation, included an obturator and complete denture in the lower jaw, normal- ized patient’s chewing, feeding and swallowing. The suc- cessful restoration of the damage functions improved his self-esteem and life quality significantly [Fig. 6]. The ap- plied method for obturator fabrication allowed easy in- sertion in the defect and shortened the adaptation period. The design of the closed substitution part of the denture allowed good oral hygiene and easy cleaning.
DISCUSSION
The prosthetic treatment of patients with maxillary resection is accompanied by numerous difficulties, as a result of violation of the septum between the oral and na- sal cavity. This imposes the use of specific methods and technologies for fabrication of appropriate prosthetic constructions. The described technique shows that the clas- sical impression methods are relevant in the cases of maxillary resection, as Zaki et Aramany claim [11]. The the- sis of some authors [8] that taking functional impressions could be possible only with special techniques was rejected. We established, that the application of classical methods, for fixing the occlusion closure and centric re- lations could be used, which coincides with the statement of many authors [21, 22, 23]. The idea that the clinical stages could be possible for implementation only with specific material and methods was not confirmed [10]. Despite the controversial opinions, it was unanimously accepted, that prosthetic rehabilitation is the optimal treatment method for patients with maxillary resection.
The described clinical case revealed that despite the defect size and the lack of teeth well planned pros- thetic construction allows successful restoration of the damaged functions. The prosthetic treatment method and the technology of the obturator were in the foundation of the achieved results. The preparation of the gypsum model before flasking provided easy and atraumatic adjustment. The hollow bulb part improved denture’s retention and stability. This confirmed the claims of some authors [18, 19] for the advantages of the closed hollow bulb obturators and rejected the views of others, that defect hermetizations is possible only with opened obturators [17, 29, 30]. The examinations confirmed the advantages of the closed obturators, as the follow up appointments showed very good oral hygiene and patient’s information, that there are no difficulties in cleaning the denture [31]. The successful prosthetic rehabilitation retrieved patient’s self-esteem and his social activity, which accord- ing to many types of research has the main role for life quality improvement [2, 4, 5].
CONCLUSION
The prosthetic rehabilitation of patients with max- illary resection is a very complicated multi-stage process, correlated with many difficulties and problems. Due to the variety of defects and clinical cases, there is no universal treatment method. This requires the research and modifi- cation of different methods and techniques, which have to provide optimum restoration of the damaged functions and to improve patients’ life quality.
REFERENCES:
- Kamiyanagi A, Sumita Y, Ino S, Chikai M, Nakane A, Tohara H, et al. Evaluation of swallowing ability us- ing swallowing sounds in maxillec- tomy patients. J Oral Rehabil. 2018 Feb;45(2):126-131. [ PubMed] [CrossRef]
- Ali MM, Khalifa N, Alhajj MN. Quality of life and problems associ- ated with obturators of patients with maxillectomies. Head Face Med. 2018 Jan 5;14(1):2. [PubMed] [CrossRef]
- Flores-Ruiz R, Castellanos- Cosano L, Serrera-Figallo MA, Gutiérrez-Corrales A, Gonzalez-Mar- tin M, Gutiérrez-Pérez JL, et al. Evo- lution of oral cancer treatment in an Andalusian population sample: Reha- bilitation with prosthetic obturation and removable partial prosthesis. J Clin Exp Dent. 2017 Aug 1;9(8): 1008-1014. [PubMed] [CrossRef]
- Artopoulou II, Karademas EC, Papadogeorgakis N, Papathanasiou I, Polyzois G. Effects of sociodemogra- phic, treatment variables, and medical characteristics on quality of life of patients with maxillectomy restored with obturator prostheses. J Prosthet Dent. 2017 Dec;118(6):783-789. [PubMed] [CrossRef]
- Chen C, Ren WH, Huang RZ, Gao L, Hu ZP, Zhang LM, et al. Qual- ity of Life in Patients After Maxillec- tomy and Placement of Prosthetic Ob- turator. Int J Prosthodont. 2016 Jul- Aug;29(4):363-8. [PubMed]
- Mittal M, Sharma R, Kalra A, Sharma P. Form, Function, and Esthe- tics in Prosthetically Rehabilitated Maxillary Defects. J Craniofac Surg. 2018 Jan;29(1):8-12. [PubMed]
- Devlin H, Barker GR. Prosthetic rehabilitation of the edentulous pa- tient requiring a partial maxillectomy. J Prosthet Dent. 1992 Feb;67(2):223-[PubMed] [CrossRef]
- Park JH, Lee KS, Lee JY, Shin SW. Fabricating a Maxillary Obtura- tor Using an Intraoral Digital Impres- sion: A Case History Report. Int J Prosthodont. 2017 May-Jun;30(3): 266-8. [PubMed]
- Bhochhibhoya A, Acharya B, Rana SB, Sharma R, Maskey B. A Sim- plified Approach for Fabrication of a Lightweight Individualized Impression Tray with the Aid of Existing Obturator Prosthesis Using Lost Salt Technique. J Prosthodont. 2017 May [Epub ahead of print] [PubMed] [CrossRef]
- Knudson RC, Williams E, Montalvo R. Stabilized record base for maxillary removable partial den- ture obturator. J Prosthet Dent. 1989 Feb;61(2):247-248. [PubMed]
- Zaki HS, Aramany M. Open- face custom tray for edentulous obtu- rator impression. J Prosthet Dent. 1981 Jun;45(6):639-42. [PubMed]
- Mawani DP, Muddugangadhar BC, Das A, Kothari V. Flasking tech- nique with alum crystals for fabricat- ing definitive hollow bulb obturators. J Prosthet Dent. 2017 Dec 16. pii: S0022-3913(17)30640-6. [PubMed] [CrossRef]
- Tasopoulos T, Kouveliotis G, Polyzois G, Karathanasi V. Fabrica- tion of a 3D Printing Definitive Ob- turator Prosthesis: a Clinical Report. Acta Stomatol Croat. 2017 Mar; 51(1):53-58. [PubMed] [CrossRef]
- Haider KG, Lewis GR. A den- ture replication technique following partial maxillectomy: a case report. Quintessence Int. 1994 Jan;25(1):23- [PubMed]
- Sukumaran P, Fenlon MR. Two-piece obturator using “lock-and- key” mechanism. J Indian Prosthodont Soc. 2017 Apr-Jun;17(2):207-211. [PubMed]
- Mohamed K, Mani U, Sarava- nakumar P, Kumar SP, Arunachalam R. Split Hollow Bulb Obturator to Reha- bilitate Maxillary Defect: A Case Re- port. Cureus. 2016 Jun 9;8(6):e635. [PubMed]
- Oh WS, Roumanas E. Optimi- zation of maxillary obturator thick- ness using a double-processing tech- nique. J Prosthodont. 2008 Jan;17(1): 60-3. [PubMed]
- Rani S, Gupta S, Verma M. Hollow Bulb One Piece Maxillary Definitive Obturator – A Simplified Approach. Contemp Clin Dent. 2017 Jan-Mar;8(1):167-170. [PubMed]
- Worley JL, Kniejski ME. A method for controlling the thickness of hollow obturator prostheses. J Prosthet Dent. 1983 Aug;50(2):227-9. [PubMed]
- Knapp JG. A simplified ap- proach to the fabrication of a maxil- lary hollow obturator prosthesis. J Prosthet Dent. 1984 Jan;51(1):67-69. [PubMed] [CrossRef]
- Jhanji A, Stevens ST. Fabrica- tion of one-piece hollow obturators. J Prosthet Dent. 1991 Jul;66(1):136-22 [PubMed]
- Schneider A. Method of fabri- cating a hollow obturator. J Prosthet Dent. 1978 Sep;40(3):351. [PubMed] [CrossRef]
- Matalon V, LaFuente H. A sim- plified method for making a hollow obturator. J Prosthet Dent. 1976 Nov;36(5):580-2. [PubMed]
- Minsley GE, Nelson DR, Rothenberger SL. An alternative method for fabrication of a closed hollow obturator. J Prosthet Dent. 1986 Apr;55(4):485-490. [PubMed]
- Habib BH, Driscoll CF. Fabri- cation of a closed hollow obturator. J Prosthet Dent. 2004 Apr;91(4):383-385. [PubMed]
- El Mahdy AS. Processing a hollow obturator. J Prosthet Dent. 1969 Dec;22(6):682-6. [PubMed]
- Browning JD, Kinderknecht J. Fabrication of a hollow obturator with fluid resin. J Prosthet Dent. 1984 Dec;52(6):891-5. [PubMed]
- Palmer B, Coffey KW. Fabrica- tion of the hollow bulb obturator. J Prosthet Dent. 1985 Apr;53(4):595-6. [PubMed]
- Hasanreisoglu U, Gürbüz A, Beyazova M. [Electromyographic evaluation of different types of obtu- rators constructed after maxillary resections.[in Turkish] Ankara Univ Hekim Fak Derg. 1989 May;16(1):45- [PubMed]
- Wu YL, Schaaf NG. Compari- son of weight reduction in different designs of solid and hollow obturator prostheses. J Prosthet Dent. 1989 Aug;62(2):214-7. [PubMed]
- Asher ES, Psillakis JJ, Piro JD, Wright RF. Technique for quick con- version of an obturator into a hollow bulb. J Prosthet Dent. 2001 Apr;85(4): 419-20. [PubMed] [CrossRef]
Please cite this article as: Gerdzhikov I. Methodology of prosthetic treatment in patients with maxillectomy. J of IMAB. 2018 Apr-Jun;24(2):2043-2047. DOI: https://doi.org/10.5272/jimab.2018242.2043
Address for correspondence:
Dr. Ivan Gerdzhikov, Department of Prosthetic Dental Medicine, Faculty of Dental Medicine, Medical University – Sofia, 1, St. Georgi Sofiyski blvd., 1431Sofia, Bulgaria. e-mail: ivan_ger1971@abv.bg
