Ivan Gerdzhikov1, Mariana Dimova2, Tihomir Georgiev3
- Department of Prosthetic dentistry, Faculty of Dental Medicine, Medical University -Sofia,Bulgaria
- Department of Prosthetic dentistry, Faculty of Dental Medicine, Medical University-Sofia,Bulgaria
- Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Medical University-Varna,Bulgaria
ABSTRACT
Aim: The aim of this study is to track the effective- ness of prosthetic treatment with post resection dentures with solid substitute part and their role in the restoration of damaged functions.
Materials and methods: The study included 14 pa- tients (9 men and 5 women) with different size and loca- tion of defects in the upper jaw treated in the period 2010- 2016 with post resection prostheses with a solid substitute part.
The impressions were taken with irreversible hydro- colloid impression material. The prostheses were com- pleted by heat-curing acrylic with low quantity residual monomer.
The effectiveness of prosthetics was evaluated by the method of Mihaylov for both oral-nasal examination of the pressure with the device “Oronasopneumotest.”
For objectifying and assess the occlusal-articulation ratios was held computerized occlusal analysis with the sys- tem T-SCAN 8.
Results: The results showed successful obturation and sealing of defects in all patients.
It was found satisfactory recovery of the speaking function and normalization of occlusal-articulation ratios. Conclusion: The prosthetic treatment with post re- section prostheses with a solid substitute part allows suc- cessful recovery of the lost speech and chewing functions, helping to restore self esteem and social rehabilitation of patients.
Key words: palatal defects, maxillary resection, ob- turator, post resection prostheses.
Damage in the maxillofacial area, occurring after maxillary resection, inflicts serious aesthetical changes, mental problems and functional disabilities in respect of impaired mastication, swallowing, speech and breathing [1, 2]. A common opinion [3, 4, 5, 6] is that the degree of func- tional damage depends on the size and location of the de- fect. This is also confirmed by a research of Usui et al. [7, 8], who discovered lesser functional impairment in patients with smaller defects, a greater number of intact teeth and mouth opening greater than 20mm. Analogous is Devlin et Barker [9] position, who found that the localization of the defect, it’s size, and the condition of the remaining denti- tion are crucial for determining the degree of functional damage and for the prognosis the treatment.
Prosthetic methods of treatment are of prime impor- tance in complex treatment and rehabilitation in patients with maxillary resection (10, 11). According to the volume of the maxillofacial area engaged, treatment has its specif- ics, with respect to the degree of disability [12].
Scientific literature describes a multitude of methods and modifications for treatment of patients with maxillary resection [13, 14, 15]. Some of these advocate treatment with closed obturators and others prefer hollow bulb obturators [16, 17]. Whatever the clinical approach, the main point of the treatment is to restore the masticatory function [18, 19]. For its improvement and for heightening of the masticatory function Umino et al. [20] suggest restoring of the occlusal contacts of first and second molars. Through videofluoroscopic analysis Yonthcev et al. [5] visualize the leading role of these molars in the masticatory cycle along with the negligible contribution of incisors and the teeth on the side of the defect. In a similar research before and after prosthetic treatment of patients with single-sided defects Xing et al. [21] found a 59,98% raise in masticatory effec- tiveness one month after the end of treatment. Similar re- sults were obtained by Vergo et Chapman [4], who improve nutrition by distributing the masticatory stress.
MATERIALS AND METHODS
With the method applied, a prosthetic rehabilitation of 14 patients (9 men and 5 women) with oncologic opera- tions of the maxilla, treated between 2011 and 2016 with closed post resection prostheses was carried out. The pas- sageway defects which occurred, were unilateral and en- gaged only the hard palate and the alveolar crest, with the natural teeth preserved (Fig. 1).
Fig. 1. Intraoral view of a patient with unilateral max- illary defect.

The prosthetic rehabilitation was carried out in 4 clinical stages. In the first one we took impressions of both jaws with irreversible hydrocolloid impression material and to avoid it’s free entry we tamponed the defects with gauze. In the second clinical stage we determined the vertical di- mension of occlusion and fixed the centric position with wax rims and light curing baseplates. After a successful clini- cal trial of the teeth in wax, the prostheses were finished in heat curing acrylic plastic with a low level of residual monomer. The cleaned and polished closed obturators with solid substitute part (Fig. 2a) were adjusted and articulated in the last clinical stage (Fig. 2b).
Fig. 2. Closed obturator with solid substitute part (a), adjusted in the patient’s mouth (b).


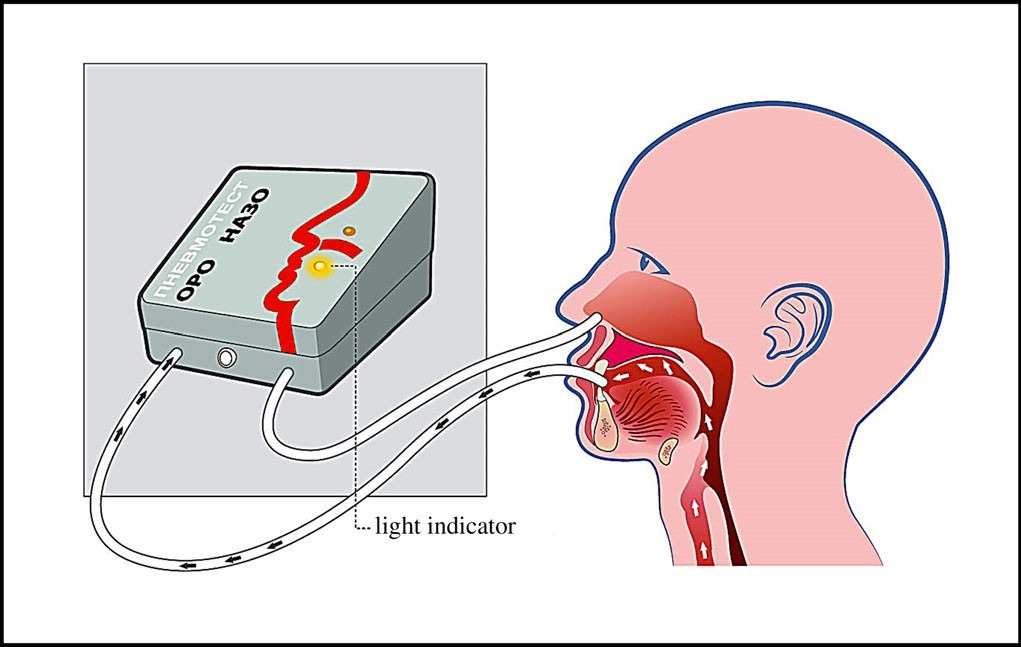
Through Mihailov’s method of simultaneous oral and nasal cavity pressure measuring, we checked the effective- ness of the reached hermetization with the “Oronasopneumotest” gauge (Fig. 3) With one of the ducts the air pressure in the mouth was gauged by the oral light indicator and the other was fixed to the patient’s nostrils by a dough consistency silicone mass to affect the nasal light indicator. With each of the patients a triple examination was conducted, where a flashing of the respective indicator read presence or lack of hermetization between the oral and the nasal cavity.
Fig. 3. “Oronasopneumotest” gauge.
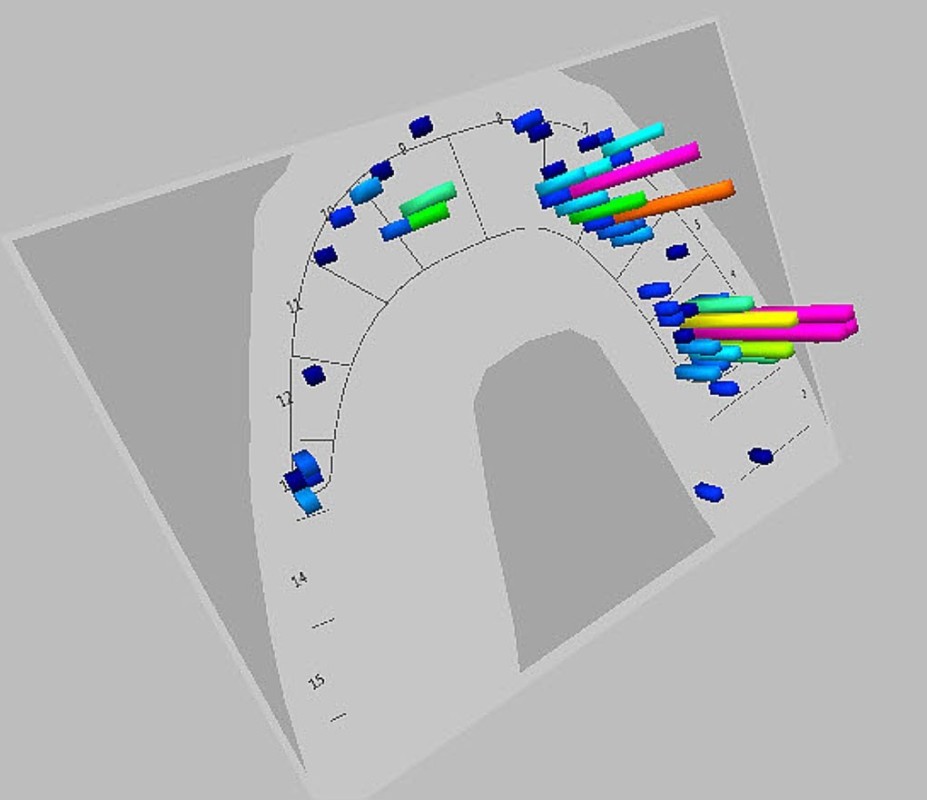
To objectify the obtained occlusal reflections, a com- puterized occlusal analysis with the T-SCAN 8 system was conducted.
RESULTS
The obtained results indicated an optimal degree of hermetization in all treated patients. The “Oronasopneumo- test” examination found a successfully created barrier between the oral and nasal cavity. The achieved effectiveness was a result of the implemented treatment method in which forming of a closed substitute part provided good retention and sufficient stability of the prostheses. Vital for the good clinical results were the comparatively small diameter and the unilateral location of the defects, as well as the presence of natural teeth.
Hermetization of postresection defects gave the opportunity to normalize the speech, mastication and swallowing in all of the patients. To the extent possible, occlusal relations were restored and documented by a computerized occlusion analysis with the T-SCAN 8 system (Fig. 4). The effect of the conducted prosthetic rehabilitation was restored self-confidence and social activity of the patients.
Fig. 4. Computerized occlusal analysis with the T- SCAN 8 system
DISCUSSION
Prosthetic treatment with post resection prostheses is the most commonly used treatment method in patients with maxillary resection [1, 2, 3]. Well-designed post re- section prostheses for maxillary defects were applied not only to maintain durable and good retention, stability, and support, but also to relieve pain and result in ease of use [11]. One of the most crucial parts in the application of ob- turator prostheses is retention. [4]. The volume and con- figuration of the defect, positioning of the remaining soft and hard tissues, and weight of the prosthesis are the ma- jor factors influencing the retention and stability of the prosthesis [8, 9].
In literature there is a multitude of methods for pro- duction of obturators, in which different materials and tech- niques are used [15]. Most authors recommend treatment with hollow bulb obturators, which reduces the volume and weight of the prostheses and aids their placement in the defect. Their main disadvantages have to do with worsened hygiene and risk of developing a bacterial infection. To overcome this, we applied prosthetic treatment with post resection prostheses with solid substitute part. The obtained results indicated good retention and stability of the pros- theses, which ensured optimal hermetisation of the defects. The positive results were due to the comparatively small defects, taking up only the hard palate and the alveolar crest, with remaining natural teeth of the upper jaw. The applied prosthetic treatment confirmed the statement, that post resection prostheses ensure the successful restoration of speech and masticatory function. The computerized oc- clusal analysis with the T-SCAN 8 system indicated nor- mal occluso-articulatory relations and confirmed the state- ment of Vergo et Chapman [4], that the even distribution of masticatory pressure significantly improves nutrition.
CONCLUSIONS
The most challenging part in rehabilitating the pa- tient with maxillectomy is achieving adequate retention and stability of the prosthesis. The prosthetic treatment with post resection prostheses with a solid substitute part allows successful recovery of the lost speech and chewing functions, helping to restore self esteem and social reha- bilitation of patients.
REFERENCES:
- Depprich R, Naujoks C, Lind D, Ommerborn M, Meyer U, Kübler N, et al. Evaluation of the quality of life of patients with maxillofacial defects af- ter prosthodontic therapy with obtura- tor prostheses. Int J Oral Maxillofac Surg. 2011 Jan;40(1):71-79. [PubMed]
- Lethaus B, Lie N, Beer F, Kessler P, Baat C, Verdonck H. Surgical and prosthetic reconsiderations in patients with maxillectomy. J Oral Rehabil. 2010 Feb;37(2):138-142. [PubMed]
- Keyf F. Obturator prostheses for hemimaxillectomy patients. J Oral Rehabil. 2001 Sep;28(9):821-829. [PubMed]
- Vergo TJ Jr, Chapman R. Maximizing support for maxillary defects. J Prosthet Dent. 1981 Feb;45(2):179-182. [PubMed]
- Yontchev E, Karlsson S, Lith A, Almqvist S, Lindblad P, Engström B. Orofacial functions in patients with congenital and acquired maxillary de- fects: a fluoroscopic study. J Oral Rehabil. 1991 Nov;18(6):483-489. [PubMed]
- Aramany MA. Basic principles of obturator design for partially edentu- lous patients. Part I: Classification. 1978 [classical article]. J Prosthet Dent. 2001 Dec;86(6):559-561. [PubMed]
- Usui H. [Evaluation of maxillary prosthesis for better QOL]. [in Japa- nese] Nihon Jibiinkoka Gakkai Kaiho. 1994 Sep;97(9):1643-56. [PubMed]
- Usui H, Sakakura Y, Shimozato K. [Maxillary prosthesis for better QOL- analysis of maxillary prosthesis sta- bility]. [in Japanese] Nihon Jibiinkoka Gakkai Kaiho. 1993 Apr;96(4):632-6. [PubMed]
- Devlin H., Barker GR. Prosthetic rehabilitation of the edentulous patient requiring a partial maxillectomy. J Prosthet Dent. 1992 Feb;67(2):223- 227. [PubMed]
- Chigurupati R, Aloor N, Salas R, Schmidt B. Quality of life after maxillectomy and prosthetic obturator rehabilitation. J Oral MaxillofacSurg. 2013 Aug;71(8):1471-1478. [PubMed]
- Chen C, Ren W, Gao L, Cheng Z, Zhang L, Li S, et al. Function of obturator prosthesis after maxillectomy and prosthetic obturator rehabilitation. Braz J Otorhinolaryngol. 2016 Mar- Apr;82(2):177-183. [PubMed]
- Borlase G. Use of obturators in rehabilitation of maxillectomy defects. Ann R Australas Coll Dent Surg. 2000 Oct;15:75-79. [PubMed]
- Anandakrishna GN, Sivaranjani, G. Management of Velopharyngeal Disorders. A Case Series. J Prostho- dont. 2010 Jul;19(5):397-402. [PubMed]
- Patil PG. New technique to fab- ricate an immediate surgical obturator restoring the defect in original ana- tomical form. J Prosthodont. 2011 Aug;20(6):494-498. [PubMed]
- Ariani N, Visser A, van Oort RP, Kusdhany L, Rahardjo TB, Krom BP, et al. Current state of craniofacial pros- thetic rehabilitation. Int J Prostho- dont. 2013 Jan-Feb;26(1):57- 67. [PubMed]
- Cotert HS, Cura C, Kesercioglu A. Modified flasking technique for processing a maxillary resection obtu- rator with continuous pressure injec- tion. J Prosthet Dent. 2001 Oct;86(4): 438-440. [PubMed]
- Elangovan S, Loibi E. Two- piece hollow bulb obturator. Indian J Dent Res. 2011 May-Jun;22(3):486- 488. [PubMed]
- El Fattah H, Zaghloul A, Pedemonte E, Escuin T. Pre-prosthetic surgical alterations in maxillectomy to enhance the prosthetic prognoses as part of rehabilitation of oral cancer patient. Med Oral Patol Oral Cir Bucal. 2012 Mar;17(2):262-70. [PubMed]
- Kreeft AM, Krap M, Wismeijer D, Speksnijder CM, Smeele LE, Bosch SD, et al. Oral function after maxille- ctomy and reconstruction with an ob- turator. Int J Oral Maxillofac Surg. 2012 Nov;41(11):1387-1392. [PubMed]
- Umino S, Masuda G, Fujita K. Masticatory performance with a pros- thesis following maxillectomy: an analysis of 43 cases. J Oral Rehabil. 2003 Jun;30(6):642-645. [PubMed]
- Xing GF, Jiao T, Sun J, Jiang YL. [The analysis of masticatory effi- ciency after maxillofacial prosthetic treatment for unilateral maxillary de- fect]. [in Chinese] Shanghai Kou Qiang Yi Xue. 2003 Dec;12(6):422-423. [PubMed].
Please cite this article as:Gerdzhikov I, Dimova M, Georgiev T. Efficiency of prosthetic treatment with post resection prostheses with solid substitute part. J of IMAB. 2016 Jul-Sep;22(3):1265-1268.
DOI: http://dx.doi.org/10.5272/jimab.2016223.1265
Address for correspondence:
Dr. Ivan Gerdzhikov
Department of Prosthetic dentistry, Faculty of Dental Medicine, Medical University – Sofia
1, St. George Sofiyski blvd., 1431 Sofia, Bulgaria. E-mail: ivan_ger1971@abv.bg
